芝麻开门,肝细胞!脂肪肝的救星溶血磷脂来也
来源:倍可亲(backchina.com)倍可亲特稿,科学专题 专栏作家:Lily/ 数百万年前,我们在丛林中漫游狩猎的祖先,常常眼睁睁看着猎物溜走,吃了上顿没下顿,可能未曾想到,他们的后代居然过上了脂肪摄入过多乃致肝脏负担过重的日子。脂肪肝是当今世界上最常见的疾病之一,30%的成年人患有脂肪肝,其中约25%为非酒精性肝病,5%为酒精性肝病。 脂肪肝早期通常没有任何症状,往往是常规体检中被检查出来的。但如果不给予适当的调理和治疗,脂肪肝可能会逐渐发展为伴有细胞损伤和炎症的脂肪性肝炎、肝硬化和肝癌。通常,有基础疾病患者如肥胖和糖尿病病人更容易患脂肪肝,而脂肪肝也会进一步加剧他们的代谢障碍和基础疾病。
健康的肝脏可以通过特定途径代谢脂质,其主要环节包括:从体液中摄取脂肪酸、原位脂质生成、脂质氧化分解(在线粒体、过氧化物酶体和细胞色素中完成)、和生成以微小脂肪颗粒排出胞外。正常肝细胞的脂肪代谢是平衡的,但如果肝细胞内的脂质积累超过其分解和排出能力时,就会在细胞内形成难以被细胞分解和排出的大脂滴。
脂质代谢需要大量的磷脂参与,磷脂是细胞膜的一种主要成分,脂质代谢时旧的磷脂不停地被消耗掉,代之以新生成的磷脂。 这个过程如同拆房子的旧墙,立马建新墙一样,需要许多指挥官(生物调节剂)的参与才能完成。有一个重要的指挥官叫溶血磷脂,它是有高度生物活性的细胞中间产物,在维持细胞磷脂供应、促进微小脂质颗粒的形成、和防止大脂滴的形成等方面有着关键作用。然而,问题来了,溶血磷脂是部分水溶性的,主要分布在血液等体液中,它们如何能穿透高度疏水的细胞膜进到细胞内大显神功的呢?
无需担心,我们的肝细胞缜密高效,善于开辟必需品运输通道。这事儿用科学术语来说就是,肝细胞可以在细胞膜上表达特定的转运蛋白分子来转运重要生物调节剂。2012年,新加坡杜克-新加坡国立大学医学院的David L. Silver团队发现了一种转运蛋白,名字超级复杂,叫含有 2A的主要促进子超家族结构域 (简称Mfsd2a)。研究者发现Mfsd2a主要分布在血脑屏障中,可协助DHA不停地转运到脑细胞中。Mfsd2a的转运功能引起了科研界的广泛兴趣。Silver团队最近发现,Mfsd2a在健康肝脏中含量很少,但在在营养过剩时可以充当溶血磷脂进入肝细胞的门户。他们观察到,Mfsd2a在脂肪肝患者或接受高脂肪饮食的小鼠肝中表达大幅增加,给肝脏特异Mfsd2a敲除小鼠喂食高脂肪饮食2~16周后,这些不幸的小鼠们患上了严重的脂肪性肝炎和肝纤维化,伴随着有益肝磷脂的显著减少。尽管Mfsd2a对肝功能“维稳”非常重要,它还是必需接受糖皮质激素受体的调控(地塞米松是就最常见的糖皮质激素)。
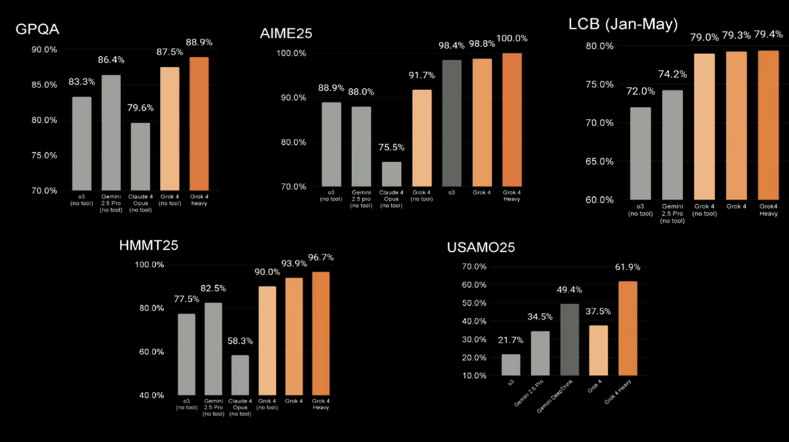
以上研究结果发表在2023年9月1日《临床研究杂志》上,标题为“Blood-derived lysophospholipid sustains hepatic phospholipids and fat storage necessary for hepatoprotection in overnutrition”(https://www.jci.org/articles/view/171267). 《临床研究杂志》一向以选稿严格、审稿时间长和审稿意见众多的而闻名,但这一研究成果因其开创性和启发性,兼有大量高质量的临床数据,被《临床研究杂志》选为 第133期的封面故事。
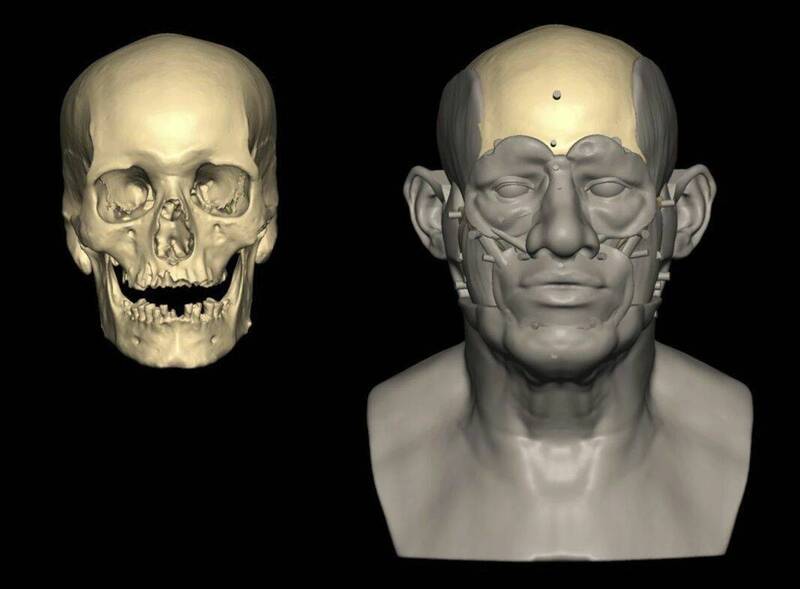
不同于在脑细胞中担任运输 DHA的中心角色,Mfsd2a 在肝细胞中更像一种临时紧急网关,正常情况下不露面,但当肝细胞营养过剩时会迅速搭建并通关。Mfsd2a仅仅在门静脉周围肝细胞的基底外侧表达,而那里正是从血液接收营养物的最前线。Silver团队还提出了Mfsd2a依赖Na+ 转运溶血磷脂的机制:Mfsd2a可能拥有V形结构,V口向外从血流中接收溶血磷脂,当溶血磷脂插入到 Mfsd2a 的疏水裂隙中后,网关就会发生构象变化,V口从向外转到向内。这样,溶血磷脂成功地从外叶转移到内叶,进入肝细胞内部。
目前,FDA 尚未批准任何的治疗脂肪肝的药物,除了维生素 E和吡格列酮分别被推荐用于治疗非酒精性脂肪性肝炎 (NASH)和糖尿病。 Mfsd2a转运溶血磷脂的这一发现可以为脂肪肝的药物开发提供很多重要启示,比如可以开发富含溶血磷脂的膳食补充剂,可筛选和测试与 Mfsd2a 结合的溶血磷脂模拟分子,可寻找Mfsd2a 特异性的GR类似分子,可合成Mfsd2a 的 mRNA 疫苗或纳米颗粒,用于替代或补充肥胖或糖尿病患者失去功能的 Mfsd2a等。
当然,脂肪肝本质上是不健康生活方式导致的,与其花大价钱打针吃药,还不如开始健康的生活方式。即使我们不再像我们的祖先那样,为了一顿饭而追逐奔跑,我们还是应该每周运动几次,对肝脏有益,也对所有器官有益。
Hepatocytes, open sesame, let lysophospholipids in to prevent fatty livers
BackChina Science Lily
Millions of years ago, when our ancestors hunted and roamed the jungle, vexed by a beast that got away so fast, moaned helplessly for the missed meal, they may never have imagined that their descendants would one day worry about consuming too much fat, burdening their livers. Fatty liver disease is one of the most common diseases in the world nowadays, affecting 30% of the adult population, roughly 25% non-alcoholic and 5% alcoholic. Fatty liver disease normally exhibits no symptoms at early stages and is often detected during routine physical examinations. However, without appropriate management and treatment, it can gradually progress to steatohepatitis (fatty liver with cell injury and inflammations), cirrhosis (liver fibrosis with built-up scars), and hepatocellular carcinoma (a form of liver cancer). Obese and diabetic populations are more susceptible to develop fatty liver disease, further exacerbating their metabolic dysfunctions and medical conditions.
A healthy liver can metabolize lipids in specific pathways, primarily involving the uptake of circulating fatty acids, de novo lipogenesis, disposing lipids through oxidation (in the mitochondria, peroxisomes and cytochromes), and exporting lipids as minuscule particles. When the accumulation of lipid in liver cells surpassed their disposal capacity, large lipid drops can form and are difficult for the cell to breakdown and eliminate. To maintain efficient lipid metabolism, phospholipids, a main component of cell membranes, are in constant demand and undergo rapid turnover in cells. This process resembles tearing down old walls in a house and immediately constructing new ones, necessitating the participation of many commanders (pathway regulators). Lysophospholipids are one of the regulators. Lysophospholipids are a group of highly bioactive intermediate cell products that play a critical role in maintaining cellular abundancy of phospholipids, facilitating the formation of tiny lipid particles, and preventing the formation of large lipid drops. However, a challenge arises: lysophospholipids are partially water soluble and primarily present in body fluids, such as blood, how can they penetrate the highly hydrophobic cell membranes to exert their functions?
Liver cells are sophisticated and swift operators. They know how to make gateways in the walls to allow essential molecules in. In scientific phrase, liver cells can express specific transporter molecules on the cell membranes. One of these transporters, with a quite complicated name, major facilitator superfamily domain containing 2A (Mfsd2a), functions as gateways for lysophospholipids to enter liver cells. Mfsd2a was identified by the David L. Silver’s team from Duke-NUS Medical School in Singapore in 2012. Mfsd2a is mainly distributed in blood–brain barrier, facilitating the transportation of DHA into brain cells. It was not considered to be a fundamental component of healthy livers. However, researchers observed that the expression of Mfsd2a increased substantively in patients with fatty livers or in mice challenged with high-fat diet. When Mfsd2a was selectively deleted from mouse livers, those unlucky rodents developed severe steatohepatitis and fibrosis after feeding high-fat diet for 2~16 weeks, associated with reduced beneficial hepatic phospholipids. Despite Mfsd2a’s potent role in transporting lysophospholipids to assist liver cells to “return to homeostasis”, its functions require the regulation from glucocorticoid receptor (dexamethasone is the most common glucocorticoid).
These significant research findings were published in the Journal of Clinical Investigation on September 1, 2023, under the title of " Blood-derived lysophospholipid sustains hepatic phospholipids and fat storage necessary for hepatoprotection in overnutrition” (https://www.jci.org/articles/view/171267). The journal of Clinical Investigation is renowned for its stringent selection process, long review time, and numerous review comments. However, this groundbreaking discovery, supported by a solid amount of high-quality clinical data, was selected as the cover story of the 133rd issue, owing to its novelty and inspiration.
Unlike its central character in brain cells where DHA transportation is constantly required, Mfsd2a acts more like temporary emergency gateways in liver cells. These gateways are scarce under normal situations but are swiftly “constructed” when liver cells encounter overnutrition. Moreover, Mfsd2a was exclusively expressed on the basolateral side of periportal liver cells, meaning the gateways open to the very front line to receive nutrients from blood vessels. The Silver team has also proposed the mechanism by which Mfsd2a transports lysophospholipids into cells in a Na+-dependent manner: Mfsd2a maintains a V-shape structure and the outward-facing configuration allows it to receive lysophospholipids from the bloodstream. Once lysophospholipids are inserted into the hydrophobic cleft of Mfsd2a, the gateways undergo a conformational change from outward-facing to inward-facing. As a result, lysophospholipids are transferred from the outer leaflet to the inner leaflet and successfully transported to the interior of liver cells.
Currently, there are no FDA-approved medications for fatty liver disease, except for vitamin E and pioglitazone, which are recommended for nonalcoholic steatohepatitis (NASH) and diabetes. This discovery can provide important insight on pharmaceutical development aimed at controlling fatty liver disease. These insights encompass various aspects, such as, the development of lysophospholipid-rich dietary supplements, the creation of lysophospholipid-mimicking molecules binding to Mfsd2a, the exploration of GR-akin molecules specific for Mfsd2a, and mRNA vaccines or nano particles to overexpress Mfsd2a in obese or diabetic patients to restore dysfunctional Mfsd2a.
Nonetheless, fatty liver disease is fundamentally related to lifestyles. It is more essential to shift toward healthy lifestyles rather than investing thousands of dollars in medications. Even if you do not need to chase for a meal like our ancestors did, it is advisable to engage in regular physical activity several times each week. This is beneficial not only for your liver but for all your organs.